Close Contact Behavior-based COVID-19 Transmission and Interventions in a Subway System
4China Electric Power Planning and Engineering Institute 5Tsinghua University
Abstract
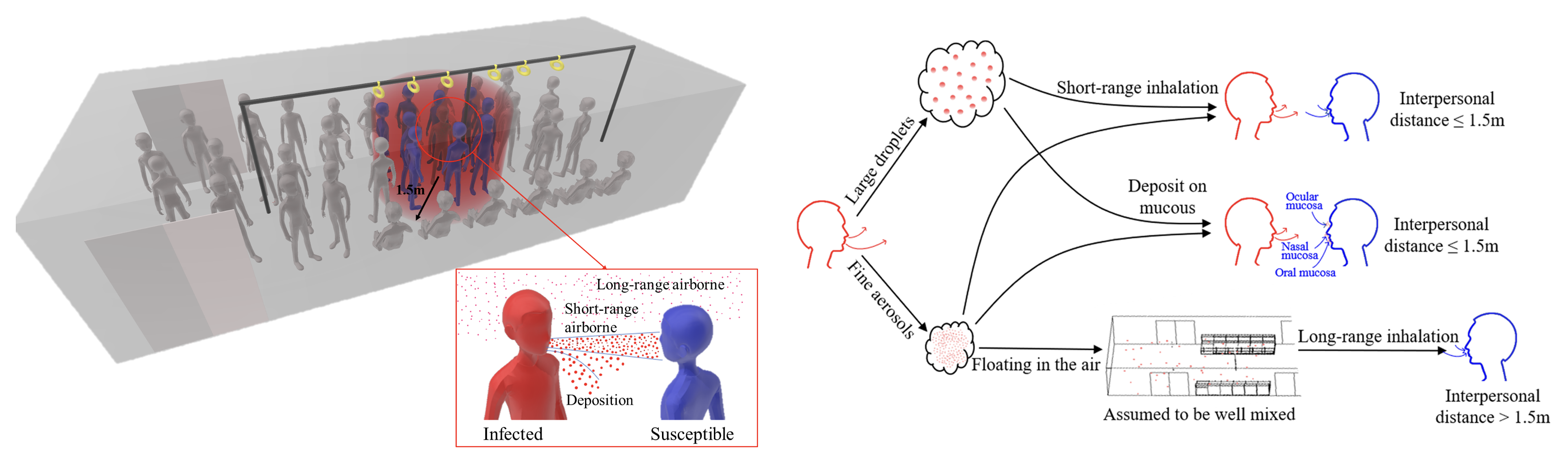
During COVID-19 pandemic, analysis on virus exposure and intervention efficiency in public transports based on real passenger’s close contact behaviors is critical to curb infectious disease transmission. A monitoring device was developed to gather a total of 145,821 close contact data in subways based on semi-supervision learning. A virus transmission model considering both short- and long-range inhalation and deposition was established to calculate the virus exposure. During rush-hour, short-range inhalation exposure is 3.2 times higher than deposition exposure and 7.5 times higher than long-range inhalation exposure of all passengers in the subway. The close contact rate was 56.1 % and the average interpersonal distance was 0.8 m. Face-to-back was the main pattern during close contact. Comparing with random distribution, if all passengers stand facing in the same direction, personal virus exposure through inhalation (deposition) can be reduced by 74.1 % (98.5 %). If the talk rate was decreased from 20 % to 5 %, the inhalation (deposition) exposure can be reduced by 69.3 % (73.8 %). In addition, we found that virus exposure could be reduced by 82.0 % if all passengers wear surgical masks. This study provides scientific support for COVID-19 prevention and control in subways based on real human close contact behaviors.
Passengers’ close contact behaviors in subway
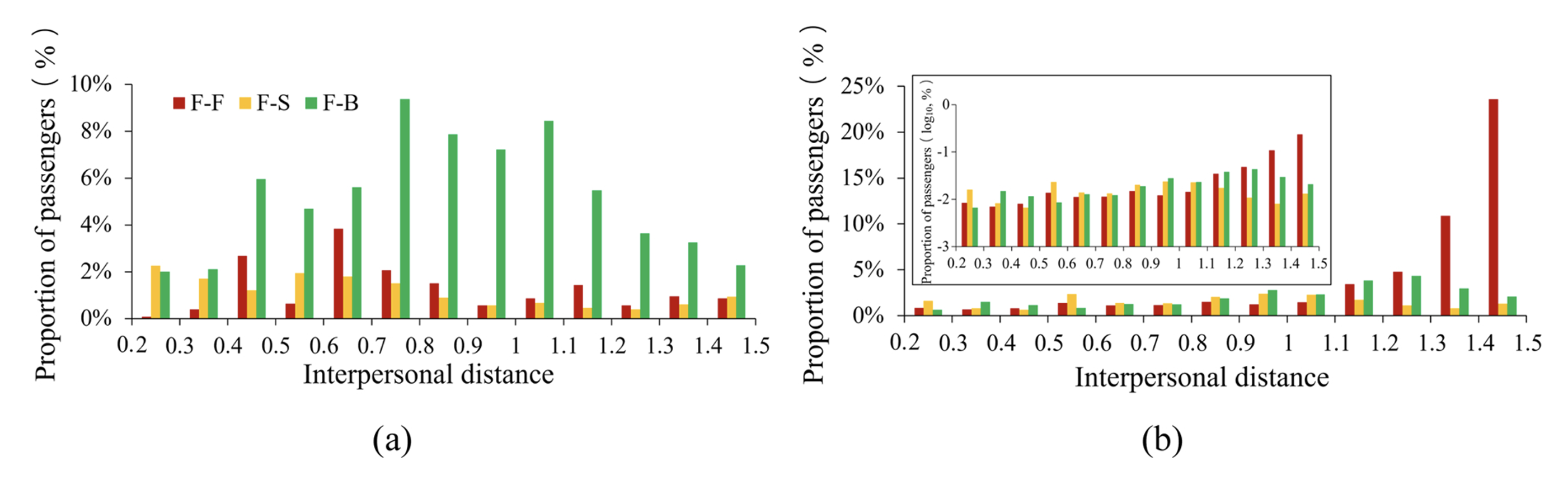
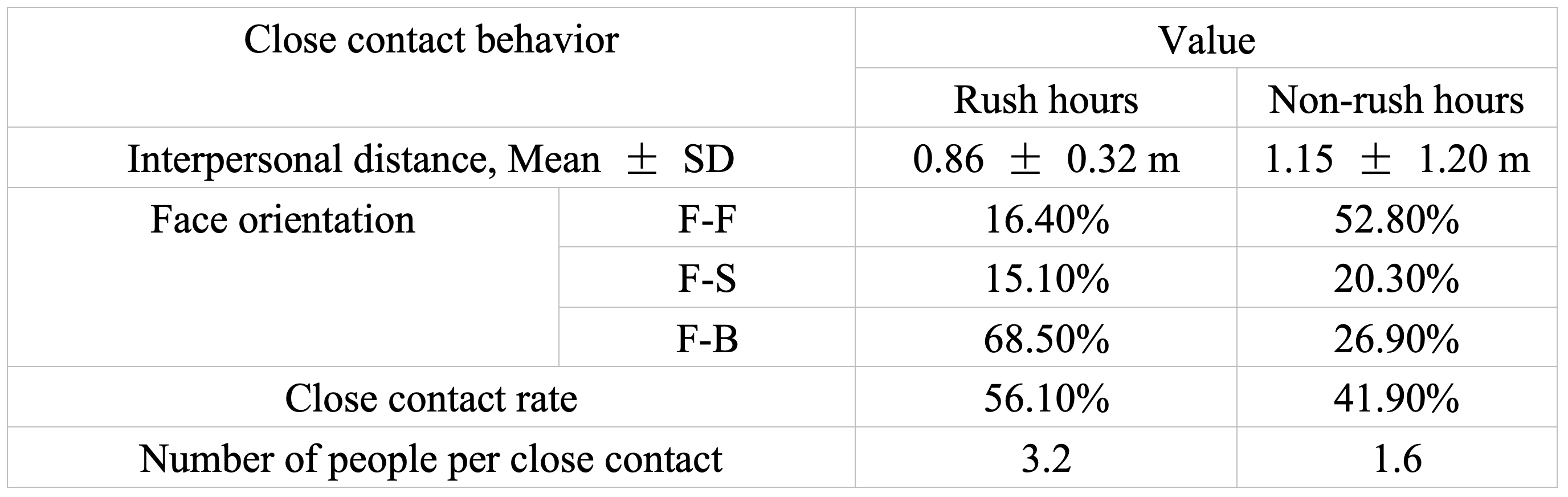
A total of 53,487 data points of close contact behavior during non-rush hour, and 92,334 during rush hour, were obtained. We calculated the probability distribution of interpersonal distance and face orientation based on all the obtained data. The average interpersonal distance was 0.8 m and 1.1 m during rush and non-rush hour periods, respectively. The close contact rate during rush and non-rush hour periods were 56.1 % and 41.9 %, respectively. The number of people per close contact was 3.2 during rush hour and 1.6 during non-rush hour. For all close contacts, during rush hour, face-to-face (F-F), face-to-side (F-S), and face-to-back (F-B) patterns accounted for 16.4 %, 15.1 %, and 68.5 %, respectively; during non-rush hour, F-F, F-S, and F-B accounted for 52.8 %, 20.3 %, and 26.9 %, respectively. All close contact behavior data are shown in Table .
Virus exposure via three transmission routes
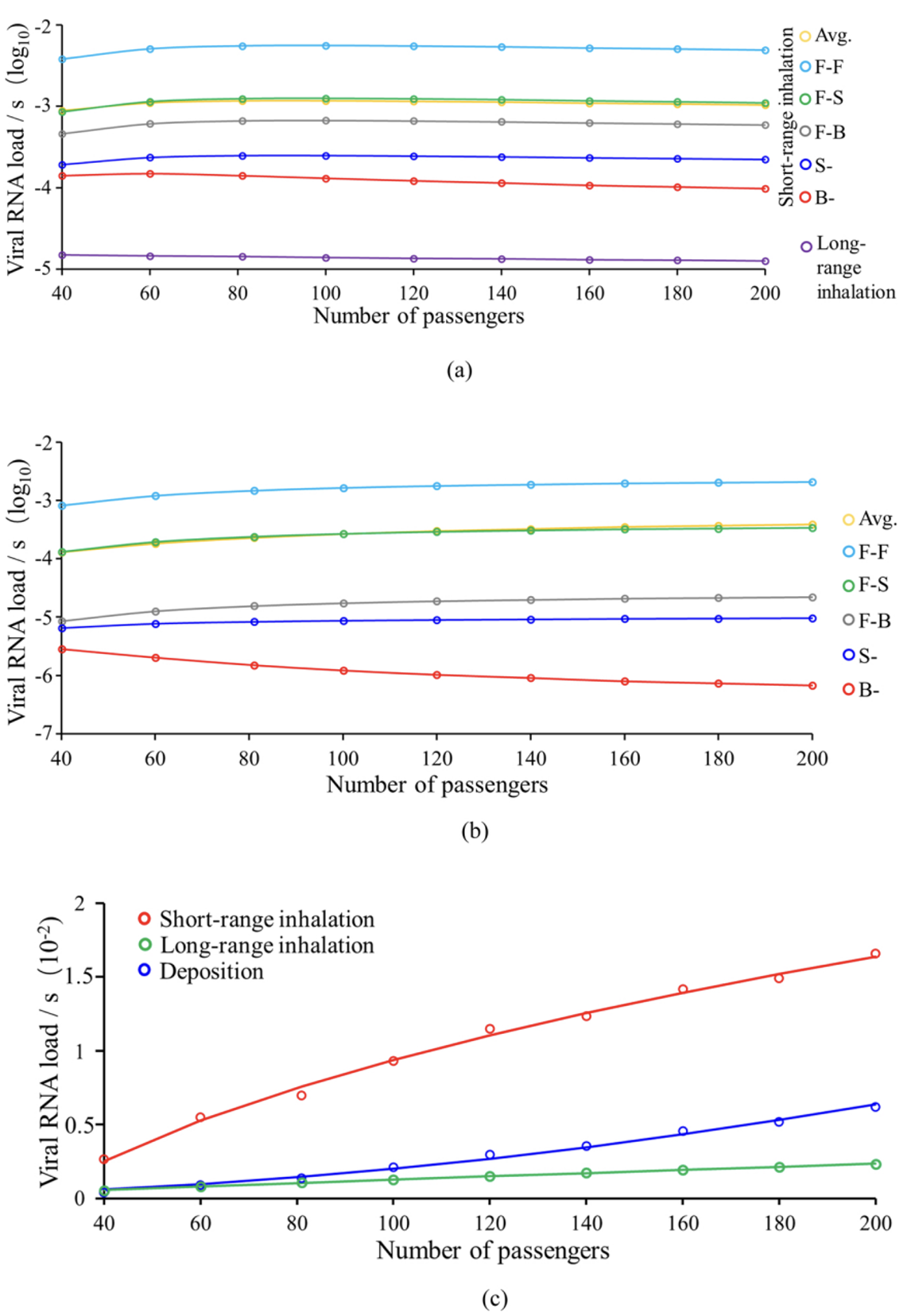
Face-to-face position resulted in the highest personal virus exposure, followed by face-to-side, face-to-back, side of the infected, and back of the infected. The virus exposure is highest through short-range inhalation, which is 3.2 and 7.5 times higher than deposition and long-range inhalation during the rush hour, respectively, and 5.6 and 3.7 times higher than deposition and long-range inhalation during the non-rush hour, respectively. The personal virus exposure through short-range inhalation, long-range inhalation, and deposition during the rush hour were 1.7, 0.9, and 2.6 times higher than during the non-rush hour, respectively. Short-range inhalation was the most sensitive to the number of passengers, while long-range inhalation was the least sensitive. During rush hour, the total exposure via short-range inhalation, long-range inhalation, and deposition were 7.1, 3.5 and 12.4 times higher than during the non-rush hour.
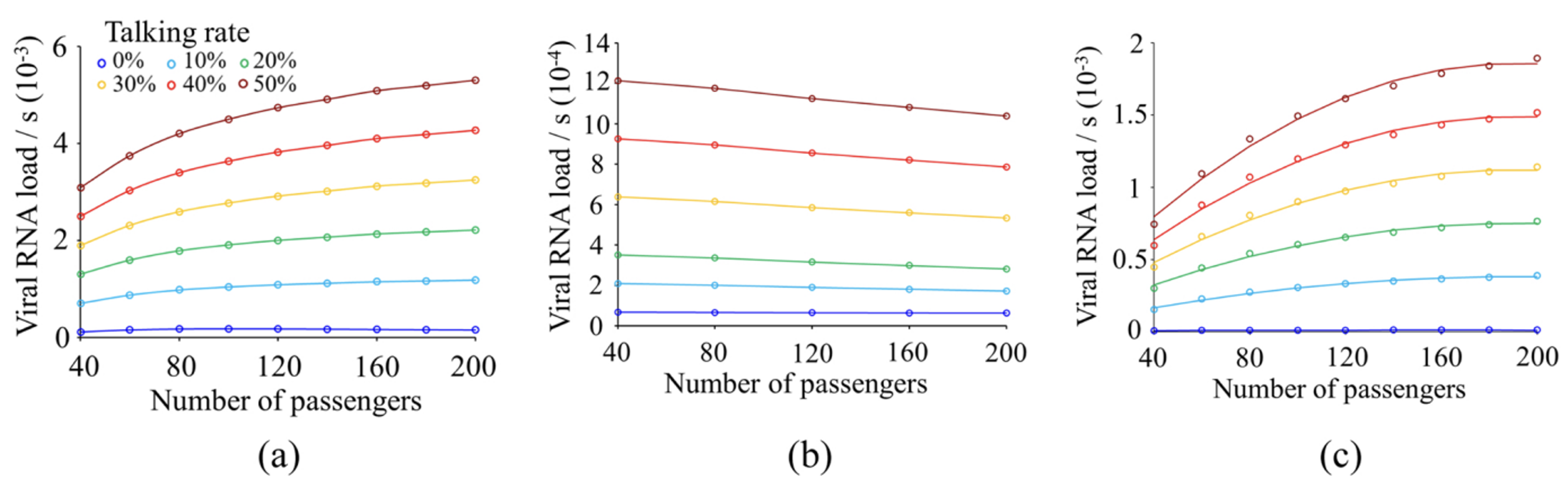
Virus exposure velocity per person via three transmission by rate of talking during close contact
During rush hour, when the talk rate is 50 %, the personal virus exposure for short-range inhalation and deposition was 31.6 and 159.8 times higher than those when the talk rate is 0 %, respectively. For long-range inhalation, the personal virus velocity during rush hour was 10.2 times higher than that during non-rush hour. Compared to the no-talk condition, when the talk rate is 20 %, the personal virus exposure and total exposure for short-range inhalation, long-range inhalation, and deposition were 1.7, 0.9, 2.7 times during rush hour, and 8.0, 3.4, 12.6 times during non-rush hour, respectively.
Interventions to reduce virus exposure
Mask
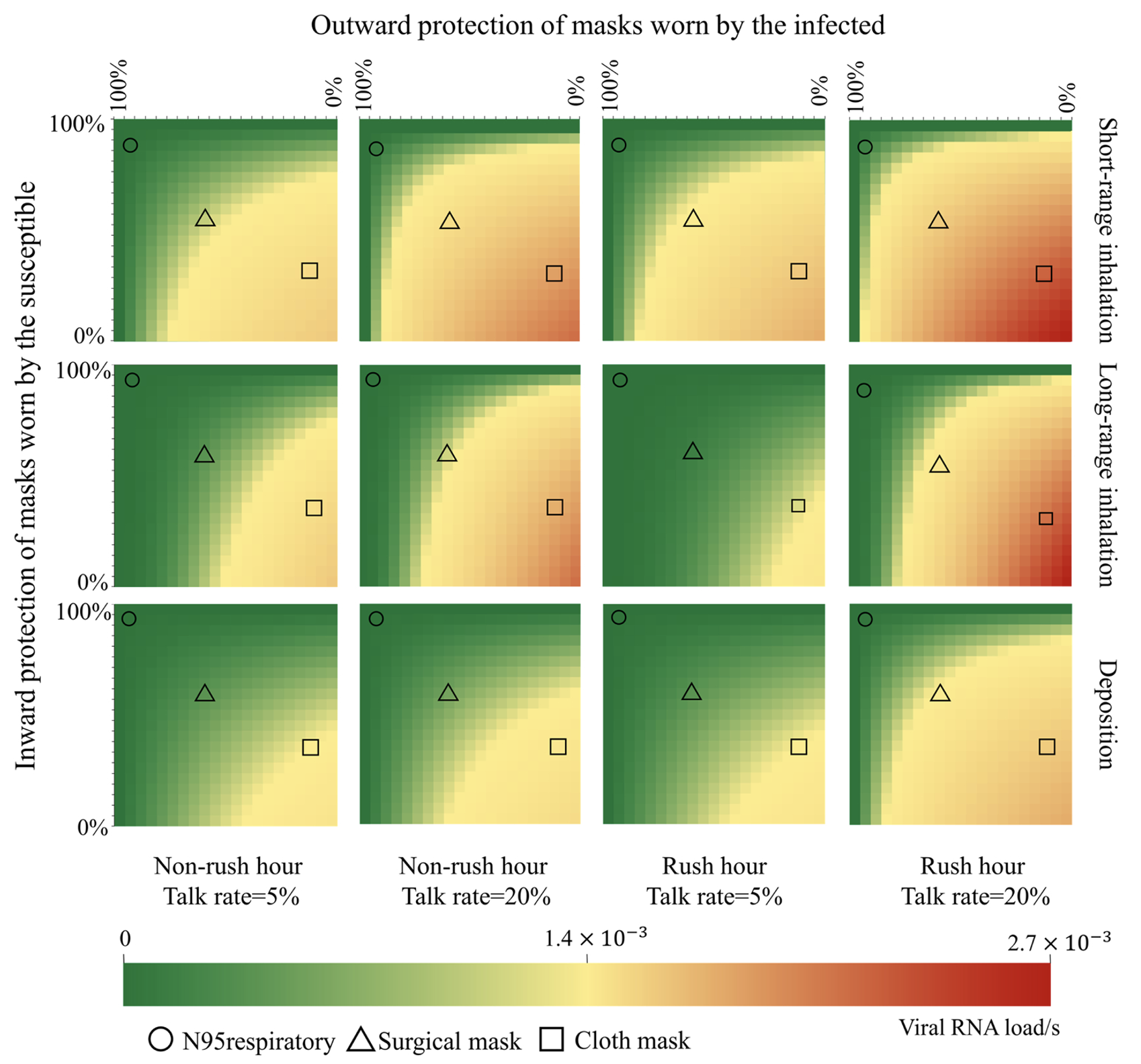
During the rush hour with a talk rate of 20 %, personal exposure was reduced by 99.5 %, 82.0 % and 41.5 % times if all passengers wore N95 respirators, surgical masks, and cloth masks (without filtration layer), respectively, when compared to no-masking. The short-range inhalation exposure could be reduced by 95.0 % and 90.0 % if the infected and the susceptible wore N95 respirators, respectively. The infected alone wearing a surgical mask was more effective than the susceptible alone wearing a mask, and the personal exposure could be reduced by 60.0 % if the infected person was the only one wearing a mask. Due to better inhalation protection, a cloth mask worn by the susceptible only was more effective than if only worn by the infected, with personal exposure being reduced by 65 %.
Passenger position
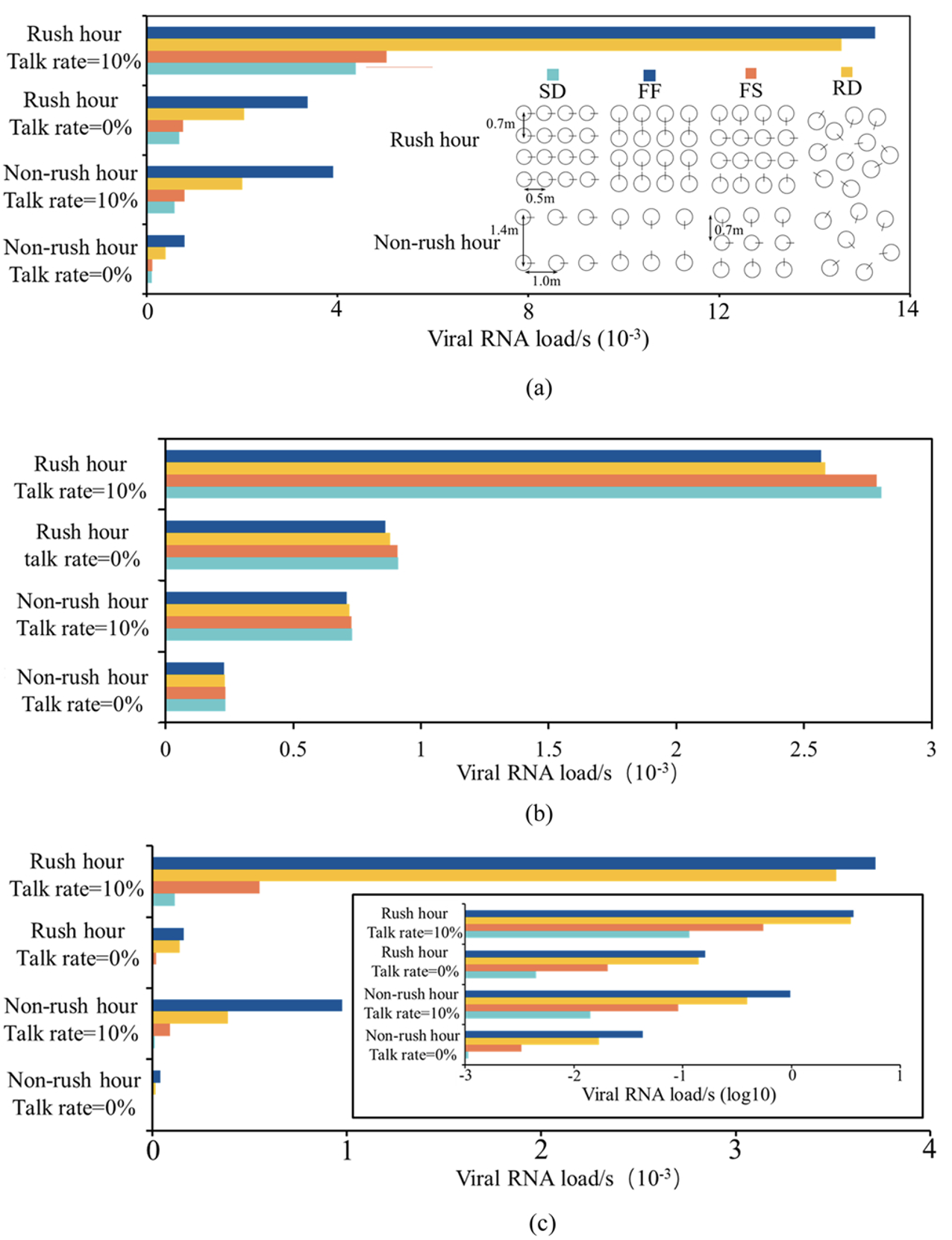
The personal short-range inhalation and deposition exposure was the lowest for SD positions, followed by FS, RD, and FF during both rush hour and non-rush hour times. When the talk rate was 10 %, the personal short-range inhalation and deposition exposure in the FF position was 3.5 and 32 times higher, respectively, than for passengers in the SD position. During rush hour and RD positions, short-range inhalation exposure was the most sensitive to talk rate, and the personal short-range inhalation exposure reduced by 86.0 % when the talk rate decreased from 10 % to 0 %, for the FS position. Deposition exposure was the most sensitive to talk rate, and the personal deposition exposure decreased by 96.3 % when the talk rate decreased from 10 % to 0 %. Changes in passenger’s relative position influences the deposition exposure the most and the long-range inhalation exposure the least. Although the long-range inhalation exposure was the highest for the FF position, the difference between the four positions was not significant.
Check out our paper for more details.
Citation
@article{liu2022close,
title={Close contact behavior-based COVID-19 transmission and interventions in a subway system},
author={Liu, Xiyue and Dou, Zhiyang and Wang, Lei and Su, Boni and Jin, Tianyi and Guo, Yong and Wei, Jianjian and Zhang, Nan},
journal={Journal of Hazardous Materials},
volume={436},
pages={129233},
year={2022},
publisher={Elsevier}
}





